Summary
Causes
- Ageing
- Previous trauma
- Overuse
- Cartilage degeneration
Symptoms
- Pain while gripping, grasping or pinching an object
- Decreased range of motion
- Decreased strength when grasping objects
- Tenderness
- Stiffness and swelling at the base of the thumb
- Enlarged or deformed appearance at the base of the thumb
Diagnosis
- Examination of the thumb
- X rays or CT scans
Treatment
- Non- Operative
- Exercise
- Anti-inflammatory medication
- Splinting of the thumb
- Ergonomic adjustments
- Surgery
- Trapeziectomy
- Ligament reconstruction tendon interposition
- Fusing the joint together
- Joint replacement
What is Thumb Arthritis?
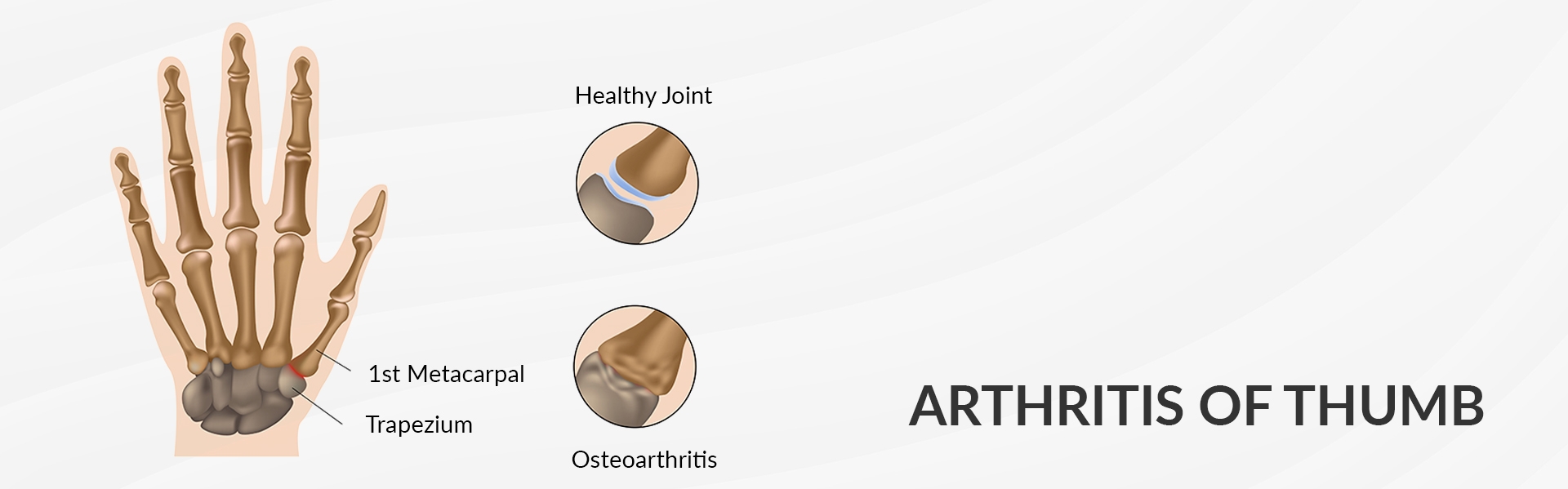
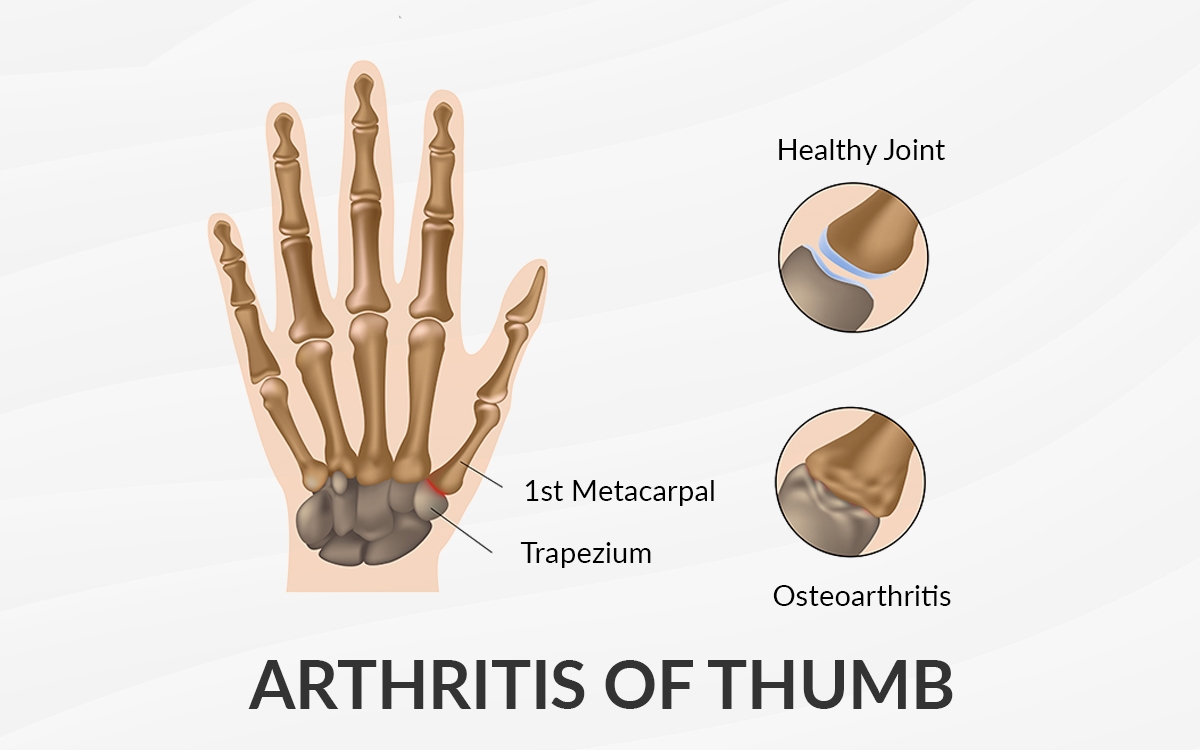
The joint at the base of your thumb enables the thumb to pinch, pivot, swivel so that you can grip things in your hand. Once arthritis happens all these motions become difficult.
Although there are several types of arthritis, the one that most often affects the joint at the base of the thumb is osteoarthritis (degeneration or wear and tear arthritis). Osteoarthritis occurs when the smooth slippery cartilage that covers the ends of bones begins to wear away.
It is more common in women than in men and usually occurs after forty years of age. Prior fractures or other injuries may increase the likelihood of developing this condition.
What is the cause of Thumb Arthritis?
Thumb arthritis commonly occurs with ageing. Previous trauma or overuse can also cause thumb arthritis. In a normal thumb, cartilage covers the end of a bone which acts as a cushion allowing the bones to glide smoothly against each other. With arthritis, cartilage degenerates and these bones then rub against each other resulting in friction and joint damage.
What are the risk factors to get Thumb Arthritis?
Factors that increase your risk of thumb arthritis include female sex, age above 40 years, injuries to your thumb joints such as sprains and fractures, diseases like rheumatoid arthritis, jobs that put high stresses on the thumb joint or overuse etc.
What are the symptoms of Thumb Arthritis?
Pain is the first and most common symptom. This will occur when you grip, grasp or pinch an object. Other signs and symptoms include decreased range of motion, decreased strength when grasping objects, tenderness, stiffness, swelling at the base of your thumb, enlarged or deformed appearance at the base of your thumb (carpometacarpal joint).
How is Thumb Arthritis diagnosed?
Your doctor will ask you questions about the level of pain, any history of a prior injury, limitations of daily function etc. They will then examine your thumb and do investigations like x rays, sometimes a scan like a CT scan.
How to treat Thumb Arthritis?
Arthritis is a progressive disease meaning it may get worse over time. There is no medication available that can slow the progression of arthritis in the thumb.
Depending on age, activity levels, the severity of arthritis and personal goals your doctor with individualise your treatment.
Non-operative treatment includes exercises to strengthen the muscles around the thumb, anti- inflammatory medications, splints to reduce stresses on the thumb on doing daily activities, ergonomic adjustments, avoiding activities that put pressure on your thumb, steroid injection etc. If these treatment options fail then your doctor will discuss surgical options with you. Depending on age, activity levels and expectations surgical options include:
- Removing a small bone in the joint called a trapezium and using a tendon to help cushion or suspend the joint alleviating pain (Trapeziectomy and Ligament Reconstruction Tendon Interposition (LRTI) using one of the tendons in your forearm).
- Simple trapeziectomy in which one of the small bones at the base of thumb known as trapezium is completely removed.
- Fusing the joint together that will take away the thumb mobility but remove the pain
- Joint replacement in which the affected joint is replaced with a metal ball and a plastic cup like a hip replacement. Though early outcomes are encouraging there are still no long term outcomes available.
What happens after surgery?
Once the anaesthetic wears off; you will go home the same day or the next depending on the complexity of the procedure. You will be given pain medications, you will be seen by a hand therapist who will make you a customised splint and discuss with you thumb and hand exercises.
Recovery will vary from six weeks to three months depending on the nature of surgery. You can drive around four to six weeks. Bigger procedures like trapeziectomy and tendon graft stabilisation or a thumb replacement, you will be able to return to your desired activities at around three months.
Are there any risks of surgery?
On the whole, the success rate is more than 95% with predictable outcomes. There are small risks which include infection, bleeding, stiffness, damage to skin nerves, dislocations, metacarpal sagging, impingement pain etc. Most patients report improved grip strength, improved function to the thumb and relief of pain. Total recovery is around nine months.
BMI Chelsfield Park Hospital
Bucks Cross Road Chelsfield ORPINGTON BR6 7RG
01689 877855
BMI The Blackheath Hospital
40-42 Lee Terrace Blackheath LONDON SE3 9UD
020 8318 7722
BMI The Sloane Hospital
125 Albemarle Road BECKENHAM BR3 5HS
020 8466 4000
Princess Royal University Hospital
Farnborough Common ORPINGTON BR6 8ND
01689 863223